A place where they do health care more cheaply and effectively. (And yes, it’s in the U.S.)
 Maple City Health Care Center in Goshen, Indiana on July 26, 2019. Photo by Chad Weaver for KHN.
Maple City Health Care Center in Goshen, Indiana on July 26, 2019. Photo by Chad Weaver for KHN.
For our Season 2 finale, time for some inspiration:
For 30 years, James Gingerich has run a super-effective clinic in Indiana, delivering great results at low cost , to high-need, low-income patients.
One is a quote from a board member that makes him sound like a big dreamer:He’s not a modest guy, and two of his brags stand out , as a study in contrasts.
“People think of us as a medical organization. We’re not. We are fundamentally a peace and justice organization that happens to be engaged in our community through medical care.”
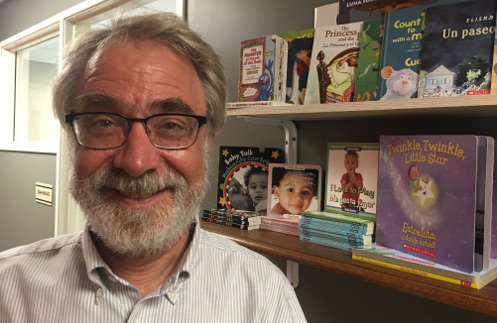
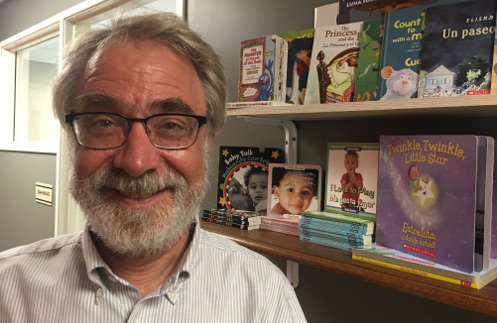
James Gingerich stands in front of shelves holding books that Maple City Health Care Center distributes to families with young children.
The other is the way he stands at his desk and nerds out on stats that show his clinic beating the pants off the competition, on preventive-care measures like screenings for cervical cancer, vaccination rates for two-year-olds, etc..
“OK, next: diabetes control,” he says. “Are you getting the idea here?”
At the heart of it, he says, is listening to people’s stories. The rest he calls “housekeeping.”
It’s not a fix for our whole broken system , you can’t just copy-and-paste what’s happening here , but it’s definitely pretty inspiring.
There’s more in this write-up I did for our pals at Kaiser Health News.
Dan: Scotian is a small city in northern Indiana, about 30,000 people. There’s a daily newspaper in English, a weekly paper in Spanish, and dozens of freight trains passing through town every day, tying up traffic. And I’m not gonna say I came looking here for solutions to the crazy price of healthcare. I’m just gonna say I came looking for signs that there might be some hope.
Maple City Healthcare Center has been here for about 30 years. It’s a neighborhood clinic. It’s a poor neighborhood. The people here are a mix of Latinos and whites, although the two groups don’t always mix. A long time ago, maple City adopted a new program for expectant moms. It’s a model developed on the East coast, and instead of just one-on-one prenatal visits, women get together in small groups that meet for a couple of hours.
The first part, they get their weight and blood pressure checked and stuff like an office visit,
James Gingerich: And then they sit around for an hour and a half talking about their pregnancies with each other.
Dan: That’s James Gingrich, maple City’s founder and medical director, and the professional staff is not there as the experts.
They are there as really group facilitators to help make sure that everybody’s voice is heard and that everybody participates. It’s a cool program, but there was a problem. We didn’t have enough Anglo women in these groups to keep an English speaking group going and a Spanish speaking group going. So we decided we were gonna do this bilingually with interpreters.
Maple City called the folks on the East Coast who created the program and said, uh, should we do this? And they said, don’t do it. It is too intrusive on the process. It’ll slow things down too much. It’ll interfere too much with, with all the real stuff that’s going on there. Don’t do it. We said, okay, we’ll do it anyway.
So we had great interpreters who were part of this. And we, we started finding that the interpretation was part of what helped the communication work well, because you could only say about a sentence worth a breath’s worth, and then you had to stop and let the interpreter interpret, and then you got a chance to think more carefully about what you’re gonna say in the next breath.
Okay? And so people started speaking with greater care and they started listening with greater care. And you got to listen twice to everything. Once in English, once in Spanish. Everything was interpreted not for the minority. Everything was interpreted for everybody. So if you spoke in English, everything was interpreted in Spanish for everybody.
And if you spoke in Spanish, everything was interpreted into English for everybody. And we got this wonderful cross-cultural stuff going on around parenting and breastfeeding and raising babies and questions going around the circle. Like, tell us about something that you, about how you were raised, that you really want to foster in this baby, that you’re expecting in this new family, that you’re expecting something you wanna continue there.
Tell us about that. Tell us about something about how you were raised that you wanna put an end to in this generation, that you don’t wanna pass along, that you wanna stop and we get all these tender, wonderful things happening, incredible things that were happening. So that was going on in the pregnancy groups.
It was a huge success.
This is an arm and a leg, a show about the cost of healthcare. I’m Dan Weissman, and it may not be obvious yet what that story has to do with cost. We’ll get there.
Maple City ended up using that experience with the pregnancy groups to address a related problem in a different part of the organization. The board of directors, the. You can already tell diversity is a big value here. And James says, when the center was getting started, the board was super diverse, culturally diverse, economically diverse, with plenty for everybody to do.
They were having hotdog sales and bake sales and trying to make these things go, and they were all engaged. And then we got to a point in organizational life where we are about executive oversight, fiscal oversight, policy oversight, all extremely middle class agenda. And before we knew it, we were left with a small, extremely dedicated board.
Extremely good people loved the healthcare center, would do anything for the healthcare center. All middle class white Mennonites do gooders. Mennonites, I should mention, Mennonites are a Christian denomination. There’s a Mennonite College in Goshen and a. Bunch of what James calls Mennonite do-gooders around.
James is a Mennonite, went to college here, got involved with some of those folks, lived in a little intentional Mennonite community in this neighborhood. He loved the experience of working with neighbors to make a stronger community, and he saw a big need for better healthcare right here, and that’s when he decided to create this clinic.
James Gingerich :I really went to medical school, not because I wanted to be a doctor, I went to medical school because I wanted to do this project. While he was in med school, he says he made sure to keep himself attached to church and community, to hold himself accountable to that vision. I’m pretty convinced that medical training is every bit as much about acculturating you into the profession as it is about actually learning medicine.
Most places in in our world, you either do well or you do good, but in medicine we had the illusion you could do both and, and so I, I wanted to to surround myself with people who would keep me from buying into that illusion. So, okay, James gets done with med school, he gets the clinic going, all this, and then years later he gets a wake up call about his board of directors while he is filling out a grant application.
And there was this question on this grant application that said, so how is the diversity of your community reflected in the diversity of your board? And he is like, Ugh, busted. So we started going back systematically and looking at where in our organization is this cross-cultural diversity stuff happening the best?
And we said it’s our pregnancy groups. So we said, now how can we reorganize our board in the image of a pregnancy group? They invited more Latinos to join the board, including folks who didn’t speak English, and they totally changed how they ran board meetings. So the question was, so how are we gonna meet that’s gonna work this way?
And we decided that the, the thing that can bind us together, that can help bring us together is narrative. So now we have a two hour board meeting once a month. Some people speak English, some people speak Spanish. We have interpreters, a few people speak both. We spend the first hour of every board meeting around a circle.
We go around the circle telling our stories around a question that’s asked. It can be something like, tell us about some time when you experienced unexpected hospitality in this community. Or Tell us about some time when you felt alienated in this community. Or Tell us about, um, how your family of origin handled money.
Or tell us about some time when you were in crisis and what did you learn about yourself? And we go around the whole circle and everybody tells their story. And it doesn’t matter whether you’re literate or illiterate, it doesn’t matter whether you speak English or Spanish. You have a story to share. And it’s an important story because part of the perspective of our community.
And that is the heart of the work we do as a board. The second hour we do what we call housekeeping. We pass budgets and policies and do all that other stuff. And we find that when we know each other this way and we know each other’s values and we understand the stories that that bring us here in our passion and why we what we care about.
The other stuff is easy. We do everything by consensus and it works.
If all this sounds ridiculously pie in the sky, impossibly beautiful. Well, let’s just take it all the way over the top. We had a board member recently say, really, we are not a medical organization. People think of us as medical organization. We’re not. We are fundamentally a peace and justice organization that happens to be engaged in our community through medical care.
You could say one organizing principle around here is to help people take care of themselves and participate in community means meeting people where they are, which means you have to know who they are. So knowing people’s stories isn’t an abstract feel good goal. It’s like the North Star for organizing the nuts and bolts, even if that connection isn’t always obvious.
Even to the folks doing it, I dunno how to explain it. It’s just, we’re more family here. We really are. That’s Diana San. She’s a medical assistant here. It’s kinda like being a nurse except then she does explain it and it is all super practical. We just do everything. We do their medication refills in house.
It sees in a hassle they’ll go into the pharmacy. The center has a stock of commonly prescribed meds. They give out for five bucks ’cause they know if a patient walks outta the doctor’s office with their medicine, they’re more likely to take it than if they have to run another errand to get it. And wonder what the price is gonna be.
Maple City also schedules doctors, so they always have time to see somebody who calls that day. And then we’re bilingual, most of us here. Right? So that’s a big help. That by itself removes a big barrier to care. ’cause if the doctor doesn’t speak your language, you gotta bring your own interpreter. Hiring bilingual staff is an intentional decision and so is having a staff of interpreters so that English only docs can see Spanish only patients.
This idea of meeting people where they are. Goes into how the staff runs their day every morning and every afternoon starts with a huddle, a 15 minute session where each medical team preps for the next few hours of appointments by zipping through the rundown and comparing notes, pooling their understanding of each case.
Okay, let’s go. I sit in on them with James’ team. Are we talking about our one 30? One 30. Mm-hmm. She had rip roaring bipolar disorder, right? Yeah. During pregnancy has been in a very incredibly stable relationship. I think her husband’s really doing great and she’s been doing remarkably well considered, but Right.
And I think you’ve, you’ve, uh, essentially I’ve given her back to you and since she’s so stable and, uh, this is gonna be a follow up almost exclusively on behavioral health issues and her bipolar disorder. Yeah. Okay. One 40. These all seem like small ways to pay attention, even obvious. But this idea of looking at people’s whole story has driven some bigger, totally not obvious decisions, for instance.
From the start serving a poor community, making care affordable, it’s been a top priority. So Maple City has always discounted services for patients with no insurance, like undocumented immigrants who can’t get Medicaid. But generally it did not do 100% free care. We’ve always wanted patients to be involved.
If it’s really good healthcare, it has to be a collaborative process, and that means that everybody has to be doing what they can. The clinic had been operating this way for almost 20 years when the 2008 financial crisis hit this area super hard, like the country’s highest unemployment rate, and all of a sudden you had families that had no source of income anymore.
You had four or five families piling it together into one house just to have a place to sleep and live, and one wage earner maybe for the whole household. The elementary school across the street started offering free lunches and free breakfast for a hundred percent of their kids. And in the midst of that $5 for an office visit, which seemed like an affordable office visit for healthcare, suddenly became prohibitive because people were foregoing food in order to come to the office.
And so people started dropping out of diabetes care. They started dropping out of wellness care. And it was, it was like it wasn’t working and we were, we’d always said, you know, our goal is to provide affordable care and ask people to do what they can. And all of a sudden we realized our care wasn’t affordable anymore for some of these people.
And it was, what do we do now? So you reduce it by another half and it’s still not gonna be affordable. So what are we gonna do? So we were sitting around the table talking about this as a staff, and somebody on the staff said, so if they don’t have money, what do they have?
And the obvious answer was time. These people aren’t employed, so they developed a new plan. Patients who couldn’t pay in cash could earn credit by volunteering for a local nonprofit for the library or wherever. Volunteer anywhere you want to, and we’ll give you $10 an hour credit on your healthcare center bill for volunteering somewhere.
You could even earn credit by investing in. Yourself. You can do parenting classes, we’ll give you credit. You can do prenatal classes, we’ll give you credit. You can work on your GED. We’ll give you credit. The point is we want to give you credit for what you’re doing to contribute to your community and your family and to your own growth.
And all of a sudden we had these people who were coming back with these coupons and with these big grins on their faces and getting reengage in care, and we knew immediately it was working. Now the people who heard about this, they were saying, so who’s underwriting all this? What? How are you writing all this stuff off?
Well, this is stuff that had already been discounted. 90%. The 10% was a little bit nothing to us. It was everything to our patients. These days, they’re taking things farther. ’cause there are some people who can’t earn those credits, like people who are too sick to do much. So Maple City is experimenting with forgiving debts.
After six months, they’ll see how it goes.
Of course, it’s one thing to offer care that’s affordable that honors people’s stories. All that’s super nice. What about outcomes? Right after this, an Arm and a Leg is a co-production of Public Road Productions and Kaiser Health News, a nonprofit newsroom that covers healthcare in America. Kaiser Health News is not affiliated with the giant healthcare provider, Kaiser Permanente.
We’ll have a little more on them at the end of this episode. So what kind of outcomes do they get at Maple City? Well, at the end of my visit this summer, James Gingrich did some of the nerdiest bragging and some of the most convincing that I’ve ever seen. We are standing in front of his computer and he starts clicking through these sets of preventive care measures.
He can compare Maple City to other clinics across the state like Maple City. These are clinics that get federal funds and serve whoever walks in the door and the other clinics. By getting their butts kicked. Like the rate of vaccinations for little kids. You can see we’re at 84. The average in the state is 27.
Jesus. Really? Yes. Or checking women for cervical cancer. And you can see we’re at 94% and the average is 51. Okay. We’re 94. He’s not done. How about colon cancer screenings? We’re at 84%. The average is 35. Okay, next is diabetes control. Okay. Are you getting the idea here? Measure after measure after measure.
So what is it that allows you to do this, that, and why isn’t anybody else doing that? So several things. From my perspective, we have relationships with patients and so they trust us and when they’re here, they’ll let us do things. Two, we have structured things in a way so that these types of, of, of labs and stuff don’t cost the patient outta pocket at all.
And then three, we try to create a schedule where we can see them when they need to be seen. Uh, and, and so the culture of collaboration and teamwork and follow up and callbacks and being flexible so that when that mom comes in with her kid who’s sick and she needs a pap smear, she’ll let us do the pap smear on the spur of the moment.
Okay, well we’ve got you right? Yeah. Uh, that makes a difference in this.
So how does all this get paid for? Well, for one thing, they don’t pay doctors a lot. James says they pay like 40% of the going rate, the going rate in Goshen. And to make that work, maple City connects ’em with a federal program to pay off their student loans, and Maple City is good at getting funding wherever it’s available, and they’re savvy about budgeting.
But it’s less about the money than the mindset. It’s this combination of commitment and creativity, the the faith that they’ll find a way. James talks all the time about a culture of sufficiency. This idea that there is enough.
I mean, I’d love to say problem solved. Let’s just put this guy in charge. I can cancel the rest of the podcast. Except no, I mean, for one thing, even here, there are limits like size. For all its creativity. The center has a limited amount of money, limited capacity for a bunch of years. Maple City basically did not accept new patients.
A few years ago, they started accepting some new federal funds and the place doubled in size, but that just confirmed something they’d already basically known. There is a limit to how big this place can get a place built on relationships, on intimacy, past a certain point, getting bigger means you lose some of that.
And take on bureaucracy and James already sees it. So when we doubled in size over the last five years, I would say we probably quadrupled in, uh, the number of meetings we have and the amount of, of that stuff that goes on. So he’s not interested in getting a lot bigger. And then there’s the fact that as invested and lovely and smart, as everybody I meet here seems to be.
There is a degree to which the whole place, the whole institution does seem to revolve around James. His vision, his energy, his commitment, his personality, and he’s about 60 years old when I talk with Don Yos, who does grant writing and communications. His title is Chief Storyteller. Of course he brings this up.
Well, we want this to continue after James, as does he. Um. It may not. And you know what, that would be okay. It would be 35 or 40 or 50 years of really good work. Um, and we could let it at that. It’s not like we’re afraid to have this place die.
That is really radical. I mean, I keep saying to people all day, nobody can just copy and paste a place like this all over the country. I mean, everything here represents custom made creative approaches tailored to this community’s needs and the actual resources at hand. So they’re not focused on building a model to fix healthcare.
They’re not even focused on building an institution that necessarily outlasts a single person. They’re just focused on making the most of the specific resources they’ve got to get the results they’re looking for right now, and it’s a constant work in progress. In other words, this place is amazing. And it’s not a solution.
And the longer I do this show, the more stories I get from you. Some many of them are just enraging, heartbreaking, horrifying, overwhelming. The more I sometimes feel like I just want somebody to fix it, and I don’t see a fix, not anytime soon.
At one point, I shared this with James and he tells me a story. A bunch of years ago, he went to a conference in California. A woman from a public housing group led a breakout session. And here’s what you said right at the top. Uh, if there’s one thing you remember, I want you to remember this. Whatever you focus on is gonna multiply.
And if you focus on the needs in your community, they’ll multiply. And pretty soon you’ll have a hundred little not-for-profit organizations all doing incredibly good work, focusing on all their little needs. And your, uh, community will remain as fragmented as it ever was, uh, and as impoverished as it ever was.
And if you focus on the small signs of hope and change. They will multiply. Um, so that inspired me to keep thinking about what is the story we wanna tell? If we wanna find stories of hopelessness, um, we can find them and they’ll multiply. Uh, and they’re out there. They’re very real. I don’t believe in denial.
And at the same time, in the midst of that, if we can find stories of. Uh, transformation and change and hope I, part of what my faith is about is that’s actually the story I wanna live into and not the other one. Yes. That in general and on this show. We are not gonna solve this thing not anytime soon, but we can absolutely be on the hunt for ways to get it to suck a little less.
Right now, we can be on the hunt for practical creative approaches and mistakes that we can learn from and for inspiration, this show’s coming back in the fall, and we’ll be looking for all of that among other things.
In the meantime, right now. You can help us by filling out our listener survey. Give us your 2 cents on what you think we should be doing. You’ll also be helping us raise money for the show. It’s a big deal, and when you get to the end, you will find a signup form for our newsletter, which I highly, highly recommend.
We’ll continue to send it out every couple weeks. In between seasons, you’ll find stories and resources and good company there, and updates about season three as we have them. That is all at arm and the leg showed. Dot com slash survey. Meanwhile, I just wanna say thank you. Thank you for listening to this show and for all of the incredible stories and insights and tips you’ve been sending my way.
We will be using them in the newsletter and to help us build season three and beyond. Thank you for being my community, for taking these stories in. Sending yours back, said from the start. This show aims to be less enraging and terrifying. And depressing than it is empowering, entertaining, and useful, and I want it to provide good company, and it is definitely doing that for me.
I hope it is at least doing a little of that for you.
Let us know. Help us get season three made. Go to Arm and a Leg Show. Dot com slash survey. I’ll see you there and we’ll be back with season three in a few months till then. Take care of yourself. This is an arm and a leg show about the cost of healthcare. This episode was produced by me, Dan Weissman. Our editor is Whitney Henry Lester.
Our consulting managing producer is Daisy Rosario. Our music is by Dave Weiner and Blue Dot sessions. Adam Raimundo is our audio wizard. Our intern is Daniel Fernandez. This season of an Arm and a leg is a co-production with Kaiser Health News. That’s a nonprofit news service about healthcare in America.
It’s an editorially independent program of the Kaiser Family Foundation. Kaiser Health News is not affiliated with Kaiser Permanente, the big healthcare provider. They share an ancestor and that’s it. It’s a fun story. You can check it out at Arm and a leg show.com/kaiser. Diane Weber is National Editor for broadcast, and Tony English is Senior Editor for Broadcast Innovation at Kaiser Health News.
They’re editorial liaisons to this show. Finally, thank you to some of our new backers on Patreon. I literally could not make this show without you. Pledge two bucks a month or more. You get a shout out right here. Thanks this week too. Dmitri Shikar. Laura Elizabeth Friddle, Jay Gardner. Jamie Hamilton Anson, Camille Carter, Lori Kraus, Suzanne Griffel, Christian Mulcahy, Ivan Meyers, John Patan, Jenna Smith, Cheryl Deval, and my brother David Weissman.
You personally bring me back to my little studio every day. It’s like you’re saying to me, it’s Thomas. Okay, let’s go.
Latest Episodes
The great American drug shortage isn’t an accident, it’s artificial (from Organized Money)
Robots sing: The Prescription Drug Playbook Song
The Prescription Drug Playbook, Part Two
Looking for something specific?
More of our reporting
Starter Packs
Help! I’m stuck with a gigantic medical bill.
The prescription drug playbook
Why are my meds so expensive?
See All Our Starter Packs
