Revisiting insulin, as relevant (and expensive) as ever
Season 4-ever – Episode 17
We’re re-releasing and updating a story we first reported in 2019, about how insulin got to be so horribly expensive, the scientists who discovered it did NOT want price or profits to keep it away from people who need it, and what some people are doing about it, today.
The story seems especially relevant right now, for two reasons:
- the COVID vaccine process has reminded all of us how vital it is to BOTH get breakthroughs in the lab AND to make sure everyone can afford to benefit from them.
- The second half of the episode, about ways that folks who need insulin are taking action on their own behalf, turns out to have been a sneak preview of this show’s current focus on self-defense.
Also, the whole thing is a wild ride. And: The updates from people we talked to in 2019? All more encouraging than we’d expected.
Send your stories and questions: https://armandalegshow.com/contact/ or call 724 ARM-N-LEG
And of course we’d love for you to support this show.
Revisiting insulin, as relevant (and expensive) as ever
Dan: Hey there. I’m bringing back an episode we did in 2019, about Insulin. For a couple of reasons.
One is, holy crap. The story we tell in the first half of this episode — of how insulin got discovered, and how it got to be so expensive— it’s just a really important and really wild story. And — in a moment when COVID vaccines remind us how important it is both to make medical breakthroughs in a lab AND to make sure that everybody can get ACCESS to them? It’s got a new resonance.
The other is: The second half of the episode looks at three ways that people who NEED insulin have mobilized for what I’d now call self-defense against insulin’s horrible price in the U.S. That’s got some extra resonance too.
We talked with three self-defense experts in 2019, and I caught up with all of them in the last week. So stick around for that at the end of this episode. OK, here we go.
Adeline Umubyeyi went to bed without dinner a few weeks ago. It’s a thing she does sometimes.
Not because she can’t afford food. Because she can’t afford insulin. She’s a Type 1 Diabetic, and if she skips dinner, she can skip a dose— and be pretty sure she’ll live through the night.
Adeline Umubyeyi: So that way I can save enough until I get my next paycheck so that I could also afford my rent, my car note this, that.
Dan:Adeline Umubyeyi’s 25, and she does not have to do this kind of thing as often as she did right after college, when she was interning with a startup. Now, she works at a law firm, and it’s a good job. With health insurance. But there’s a deductible. So in June, she’s still paying for insulin herself, about 350 dollars every four weeks.
Adeline Umubyeyi’s known since she was a teenager that the price of insulin was going to play a major role in her life. After her dad died,
Adeline Umubyeyi: We didn’t have insurance me and my mom would go, um, to, you know, the CVS. I was about 17 and they were like, you know, for her insulin, it’s going to be $ 3,000. It was so heartbreaking.I think that’s when I really realized, Holy Shit, like I’m on my own.
Dan: Like, this wasn’t something her mom could really protect her from, not for the rest of her life. Her mom found the money— it was not easy— and from then on it was a scramble: credit cards, help from relatives, from non-profits, whatever it took.
And since Adeline Umubyeyi’s been on her own she’s always found a way— including skipping doses and skipping meals. Which isn’t really safe. People die every year.
Adeline Umubyeyi: You know insulin for diabetics is like oxygen for us. We need it. If we don’t have it, we’re not going to be able to live until the next day. It’s really that simple, and that’s how I try to explain it to people.
Dan: AND YET: one out of every four Type 1 diabetics rations their insulin.
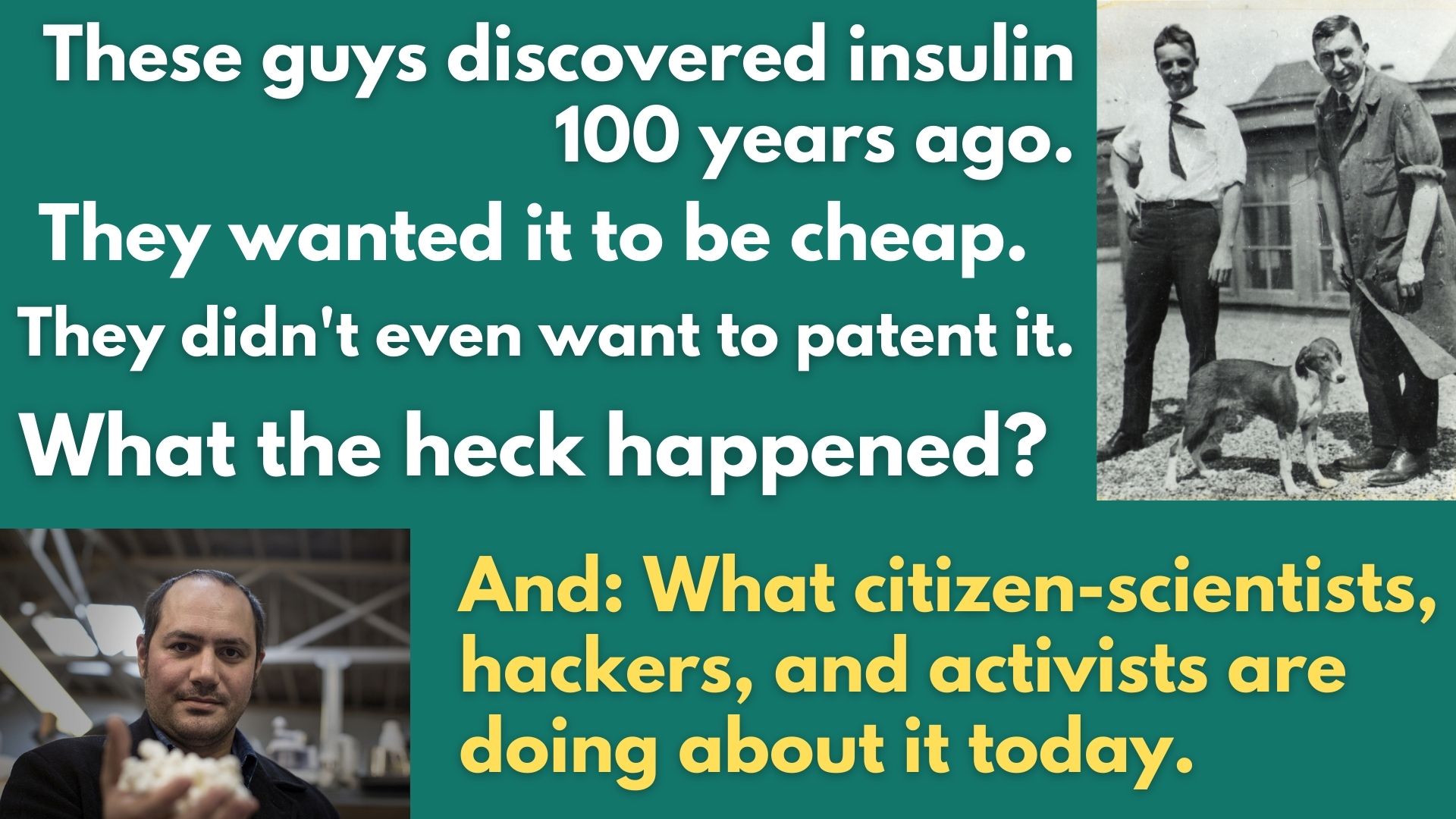
That’s hundreds of thousands of people. Buuuut… this is old-school technology! Insulin was discovered almost 100 years ago by Canadian scientists who didn’t even want to patent it; they just wanted people to have it. That story is told in an AMAZING book called “The Discovery of Insulin.” It’s got everything. Especially: scrappy, naive researchers, swatting away flies in a sweltering attic, leaving a trail of dead dogs in their wake.
And that story has a TON to tell us about how we got to this point— and where we might go from here. It may not be entirely hopeless.
This is “An Arm and a Leg,” a show about the cost of health care. I’m Dan Weissmann.
Life before insulin was stark. Here’s Jing Luo— he’s a doctor, and a Harvard researcher who studies access to insulin.
Jing Luo: Type one diabetes was a death sentence. Kind of a rough way to die.
Dan: Yeah. Unquenchable thirst, constant hunger— and a rapid wasting. Frequent bonus symptoms include blindness, itching, and boils. BOILS.All accompanied by non-stop peeing: In Greek, “diabetes” means “pipe-like”— liquid goes in one end and out the other. An English surgeon in the 1600s called it “the pissing evil.” And the urine is full of sugar.
Jing Luo: Right. Yeah, yeah. In addition to having profound thirst, drinking a lot of water, you’re peeing all the time—is that your urine was sweet.
Dan: So doctors confirmed your diagnosis with a taste test.
Early 20th century medicine had exactly ONE treatment for extending the lives of diabetics: Slowly starving them to death.
It was unbelievably grim.
Jing Luo: I find myself pausing and like wiping away tears, reading about, um, you know, for example, small nearly blind boy who’s wasting away, who they could not figure out —despite a very, very, very, very stringent starvation diet—why he was still having glucose in his urine. And it turns out that he was eating the bird feed right from his pet. You don’t— that’s like crazy. How can we do that to people?
Dan:And that was the state of the art treatment.
Jing Luo: Yeah.
Dan: And starvation only worked for so long.
Enter a struggling country doctor, Frederick Banting. Seriously struggling: He hung out his shingle in July 1920 and got NO patients for weeks. Months went by. He worried his fiance would break up with him.
Then one night, Banting got an idea that he hoped could give him his big break: finding a treatment for diabetes. He stayed up till 2 a.m. thinking about it.
At the time, scientists thought something in the pancreas might help diabetes… but something ELSE in the pancreas interfered.
Banting had a complicated idea for isolating the good stuff. Take a bunch of dogs: Make some of them diabetic by removing their pancreas.
Then raid the pancreases of the other dogs, using a dicey, untested surgical protocol he’s got in mind, to isolate the good stuff. They made a TV mini-series about this whole story in the 1980s. It shows Banting, telling a friend about his idea.
Banting: Make an extract from this pancreas and pop into the diabetic doc. Now if the diabetic dog’s, blood sugar goes down, I’ve got something!
Dan: A week after his sleepless night, Fred Banting was at the University of Toronto, pitching a big-time professor of physiology. He said: Give me a lab, a salary, and some dogs.
The professor thought Banting was kind of a rube, and his idea was kind of half-baked — but maybe not ENTIRELY worthless.
The professor said, no salary, but come back next summer and you can have some dogs and maybe a medical student to help. On May 17, 1921, Banting and that student assistant cut open their first dog.
In the next two-three months, they killed a bunch of dogs— some from diabetes, but mostly via incompetent veterinary surgery.
The movie does a great job showing them literally sweating it out— fans going, no shirts, flies everywhere — and just fumbling. Here they are, butchering another dog.
Banting: Christ. Christ Fred, I’m losing. Get an obstruction. GET A GODDAM OBSTRUCTION. OK, OK- there’s no need to shout for Christ’s sake
No go. Dog dies. There’s a long, long pause. The assistant gets up, slowly walks over and leans against a glass cabinet full of lab stuff.
Banting: I’ve never killed anything before.
Dan: So much for that cabinet…
But, for all that, they did produce some blood-test results that showed promise— hints that the stuff they were getting from dog pancreas may not be a total bust.
They got more dogs— by hook or by crook, going out and buying them on the street from— well, probably dog-nappers— and as summer ended, they managed to keep a diabetic dog alive for three weeks.
BAM. Game on. They got the university to buy them some more dogs.
In the next couple of months they learned they’d been taking long way round.
There was no need to get the pancreatic “good stuff” from surgically-treated dogs. You could just go to the stockyard and get some fresh cow pancreas— or pig, that could work too— grind it up, and go.
Next, a more-experienced guy joined the team— a biochemist named James Collip. Within a couple of months, Collip had nailed down a method for making insulin. It’s a big moment, and the mini-series really plays it up:
James Collip: I’VE DONE IT!!!
And then the really huge moment: The team tried this stuff out on a human subject— a 14 year old kid who was down to skin and bones— and it brings the kid’s blood sugar down to normal levels.
They tried it on six more patients, with good results.
A few months later— less than a year after Fred Banting cut open his first dog— they present at a big medical conference, and everyone completely. Loses. Their mind.
But by then, there were… some problems. For a couple of months that spring, they couldn’t get a decent batch of insulin made. Collip, the biochemist, was beside himself.
James Collip: You think recapturing it would be easy, especially for me. I mean, I saw it. I held it in my hands.
(There were other problems too, behind the scenes: Banting got convinced that the more-experienced scientists on the team were trying to hog all the glory. He may have beaten up Collip the biochemist. Maybe twice.)
And there are all these diabetics, starving themselves to death.
Meanwhile, a U.S. pharma company, Eli Lilly, had been tracking the insulin research in Toronto for months, sweet-talking the researchers at every opportunity.
The Toronto scientists had been putting Lilly off all this time— they did NOT want their discovery to become someone’s commercial enterprise.
But they needed someone with resources— bigger labs, more capital — to take insulin over the finish line.
So, reluctantly, the researchers called Eli Lilly and said, “Let’s make a deal.”
And the rest — you could say — is grim corporate history.
The deal the Toronto researchers made with Eli Lilly was supposed to be limited, a way to get some insulin out there while Toronto figured out a way to get more insulin made, for everybody. Lilly got an exclusive license to make and sell insulin— but just for a year.
But a year was enough to give Lilly such a head start that no U.S. company could catch up.
(And none did— the other two companies that sell insulin today are European, and also got the basic science directly from the Toronto researchers.)
In that first year, Lilly developed improvements to the insulin-making process: patentable improvements, trade secrets.
Then, over the next few decades they went on to improve insulin itself. Here’s Jing Luo again:
Jing Luo: These early products are quite rudimentary because, you know, they were large amounts of volume of liquid. You’d have to inject into your, let’s say the, the fat just by your, by your belly button, um, or on your thighs. And you’d have to do that multiple times a day. And, you know, because of impurities, you might have injection site reactions, you know, redness, inflammation, pain at where the injection is happening. or the potential allergies that may come from the fact that, um, who knows what’s in this ground up pancreas?
Modern insulin is a completely different thing.
Jing Luo: We’re not going to, to stock yards anymore looking for animal pancreases. These are all synthesized. These are more like designer and insulins, um, in the sense that, um, um, they’ve been really modified at a molecular level. It’s super cool stuff. And you know, there are, there are multiple Nobel prizes in physiology and medicine that have made this happen.
Dan: Buuuut… modern insulin it’s not new anymore— Lilly’s product, Humalog, came out in 1996. Some modern insulin isn’t even under patent protection.
So, why isn’t there generic insulin?
Jing Luo says: Basically, there are easier things to knock off.
Insulin’s harder to make than regular meds like Tylenol, and it’s in a special class of drugs for which the FDA requires especially-stringent— and especially-expensive— testing.
And then there’s this: Even though the active ingredient of brand-name insulin may not have changed, the big three companies have continued to change— and improve— the drug-delivery systems—like: wearable insulin pumps.
Patients like those pumps a LOT better than shooting up with a syringe in the belly button, and the dosing is steadier. Which means: safer.
… And there are a million patents involved in making insulin that works with those devices.
Jing Luo: Like once you add all these different layers to this thing, to the medicine itself, um, companies can stack dozens of patents on top of each other to try to thwart generic competition because they can say, look, we’ve got three patents on the active ingredient. We’ve got patents on the medical uses of the active ingredient. We’ve got patents on the nonactive, um, excipients associated with this ingredient. We’ve got multiple patents on the devices. Yeah. And so you who are trying to enter this space, we’ll sue you for patent infringement on all of them.
Dan: Jing Luo says this is standard with Big Pharma for pretty much everything
Jing Luo: So when you, like, when you listen to these like CEO’s of Pharma companies being interviewed at CNBC. Yeah. You know, they’d be like, well, what about generic competition for this product? And they’ll just keep saying, no, no, no, we’ve got this really robust patent portfolio we can with Tan withstand any challenge. We’re going to tie this up in court forever and don’t worry about it. We’re going to continue this gravy boat for a long, long time. That’s the way they reassure investors.
Dan: But the upshot is: Hundreds of thousands of people can’t afford the insulin they need to live. Which is why Jing Luo finds the book about insulin’s discovery so moving.
Jing Luo: Yeah. You know, we’ve come so far and yet we still have, um, adults dying, um, from rationing their insulin because of cost. It’s like, it’s, it’s, it’s so disheartening.
Dan: So, this story started with a group of scrappy, kind of under-resourced researchers— and it turns out, there’s a group of exactly the same kind of people working on the problem of expensive insulin today. In Oakland, California. More on that, right after the break.
This episode of An Arm and a Leg is a co-production with Kaiser Health News, a non-profit newsroom that covers health care in America. Kaiser Health News is NOT affiliated with the giant health care provider Kaiser Permanente. We’ll have a little more on them at the end of this episode.
Since 2015, volunteer researchers at the Open Insulin Project in Oakland have been working on a recipe for insulin, with the goal of sharing that recipe as widely as possible.
In an age where it’s possible to 3-D print an actual house— yah, really. Google it! — why can’t we figure out how to make our own insulin?
The project runs out of Counter Culture Labs. That’s a microbiology maker-space in what sounds like a kind of anarchist community center.
Producer Avery Trufelman lives and works nearby, and she very kindly went to check it out.
Avery Trufelman: So I just biked up from my house to Telegraph Avenue to Shattuck to Omni Commons, which is a collective of collectives. It’s totally awesome. It’s like a very cool place. Um, and in it’s in this big beautiful building and they have a theater and uh, food not bombs is here and a lot of other organizations and it’s pretty funny that this is the place where it all goes down.
Dan: Avery met the project’s founder, Anthony Di Franco.
Avery Trufelman: Hi, are you Anthony? Yeah. Hey Avery. Nice to meet you. Thank you for letting me come crash.
Anthony: Welcome.
Dan: Anthony is a Type 1 diabetic. He isn’t trained as a biochemist. He’s a computer-science guy. He does enough consulting work with those skills to stay afloat. He devotes the rest of his time to Open Insulin.
This is a lab with murals on the walls, and a bike rack by the door. One of the other projects here is an effort to make decent vegan cheese.
And even the fancier lab equipment — like a super-cold refrigerator — has … quirks.
Avery Trufelman: It is. It’s kind of funny though cause it does look like a fridge at like, um, I don’t know the house with a lot of people in it. Like there’s lots of different link which lists and handwriting and yeah, it’s very, it feels very homey. It doesn’t feel like a, yeah. Yeah. I mean it does feel like a science fridge but it feels like a communal side.
Anthony: Yeah, you don’t kind of have to feel like you’re, you’re on a movie set that has the ideal of science. You can do real science and just kind of do what you need to do.
Dan: And what Anthony wants to do in this funky little lab is to address the enormous problem of profit-driven medicine, starting with insulin.
Anthony: I think there’s really broad acknowledgement that something really terrible is wrong with the system, but we just have to like have the courage to, to name it and to propose alternatives.
Dan: Later, I get to ask Anthony some questions about their progress. He says after four years, they’ve got a process that’s producing a little bit of insulin. Next steps: Refine that process, publish it, and help other people learn to do it.
Anthony: It’s, I think it’s somewhere in the ballpark of what it takes to brew a really good beer. So I don’t think it’s something that most people can’t do. But it does require you to put the time in, and the attention in, to get it right.
Dan: So this would be like a home-brew beer kit for insulin?
Anthony: Yeah. It might be a little bit more like what you would find in a microbrewery then like a home brew kit.
Dan: He thinks a neighborhood operation — maybe in a storefront or a clinic or even a pharmacy— could serve a local community, kind of like a craft brewery. They’re starting to think about the practicalities — they’ve recruited some pro-bono lawyers, and are forming committees to write bylaws for a tax-exempt non-profit. Jing Luo, the Harvard researcher, would expect the craft-brewery model to hit a regulatory brick wall.
Jing Luo: You can’t make enough of it in a sterile enough condition at capacity in order to get the FDA who’s going to inspect your plan to say, okay, I’m going to approve you to sell this drug
You know, this is not homeopathic treatments that you can just sell at the farmer’s market because of the DEA and the FDA. They would just shut you down.
Dan: Here’s a different perspective: Jean Peccoud is a professor at Colorado State who has written about Oakland’s Open Insulin Project. He’s kind of a fan, and they claim him as an ally. He’s also skeptical about getting FDA approval for open-source, craft-brewed insulin. But he’s got his own idea: bypassing the FDA. Just like you don’t need the liquor commission’s OK to drink the beer you brew at home, you don’t need the FDA’s permission to make your own insulin.
Jean Peccoud: There is nothing that prevents the patient from manufacturing a drug for himself. You know, you can inject yourself with whatever you want.
Dan: What he imagines sounds even simpler— at least for the user— than a home-brew kit for beer.
Jean Peccoud: The level of complexity is more like making a bread machine tool for making, insulin. I mean that’s the level of complexity that we are talking about.
Dan: He tried raising money last year to get a project like that going — put out a YouTube video— but it didn’t take off. He only collected $197— half of it from his teenage kids. It just gave you money from their allowance to do it.
Jean Peccoud: Yeah, they thought it was cool.
Dan: Did you, did you, did you give it back since you’re not going forward with it?
Jean Peccoud: Yeah.
Dan: I ask Anthony DiFranco at the Open Insulin Project how he’d deal with the FDA.
Anthony: That’s a good question. I mean, all of these questions of like what, what this would count as in terms of regulation are as far as I know, open questions and we’re eagerly awaiting, uh, the opinions from our actual legal counsel
Dan: I ask him how sure he is that they’ll get it working, and practical.
Anthony: Well, what’s the deadline?
Dan: Fair question. Meanwhile, diabetics die rationing their insulin every year. And last year, Eli Lilly took in about $3 billion on insulin.
So it sounds like the score is: Eli Lilly 3 billion, scrappy researchers zero. So Far.
As I was wrapping up Season One of this show, I got an email with the subject line: “I AM PART OF A MOVEMENT.”
It was from Terri Lyman, a Type 1 diabetic in Arizona. She doesn’t make her own insulin, but she has hacked together an artificial pancreas.
Terri Lyman: I can’t even begin to tell you how different life is with it than it was without it. I would never want to be without it.
Dan: Her pancreas? It uses open-source software that ties together an insulin pump and a glucose monitor. Together, they monitor her blood sugar, and give her just the right amount of insulin to keep her at a healthy level.
Her rig uses an out-of-date pump— like from 2002— and a similarly old glucose monitor— that’s what’s hackable— and a little thing she pulls out of what I think is an eyeglasses case while we’re talking on FaceTime.
Terri Lyman: That little thing there. That’s a computer. Okay. This is the communication board.
Dan: It looks at this is like, this is like a raw motherboard. This is what the inside of my computer it looks like if I took it. Yeah.
Terri Lyman: Exactly. That’s the brain, that little silver thing. That’s the communications. That’s where all the antennas are. Cause it’s got Wifi, Radio Frequency and Bluetooth…
Dan: Since she put her system together, the company Medtronic has come out with a machine that does similar things. Her doctor keeps asking her if she wouldn’t like to switch. She keeps telling him no.
Terri Lyman: that new pump is hugely expensive and it doesn’t do half what this does.
Dan: She has customized her system to give her more information— hour by hour, day by day— about how her body processes glucose and insulin— and more control. It took a lot of work.
Terri Lyman: I built my system over the course of a year, I was learning how to program computers. I mean that process for me was long and slow. I’m 53. I am not a spring chicken and learning to code is tough
Dan: She succeeded because there were other people out there doing the same thing: a community, a movement.
Terri Lyman: every time I needed help, there was somebody online who could answer my question or could tell me where to read it. No, you’re on the wrong page. Go to this page. No, you don’t do it that way. You do it this way.
Dan: She shows me the real-time readouts of her blood sugar, insulin levels— all kinds of thingsI tell her the whole thing seems pretty overwhelming.
Terri: And yeah, it is a lot of commitment, but diabetes isn’t for the weak (Laughs)
Dan: The community around these tools is bigger than when she started. The tools are easier to use.
Dan: She says the big medical companies haven’t taken legal action to stop them.
Terri: They uh, called US names. The big ones were rogue cowboy hackers. That was one slur — which we were overjoyed: We’re rogue cowboy hackers
Dan: That’s exactly what Anthony Di Franco wants to be for insulin. It’s what Fred Banting was. We need rogue cowboy hackers to combat— or at least complement— the Eli Lilly’s of the world.
And there are other ways to be part of a movement. Remember Adeline Umubyeyi Umubyeyi from the beginning of our show? She has started volunteering with a group called T1 international that advocates for Type 1 diabetics.
Around the same time she talked with me, she told her story to more than a dozen members of Congress at an event in DC.
Adeline Umubyeyi: I hope that I can help cause a spark and create a change.
Dan: Me. Too.
So, that’s where we left things in the summer of 2019, with our three self-defense experts: Adeline Umubyeyi Umubyeyi, the budding activist in DC. Terri Lyman, the rogue cowboy hacker, with her open-source insulin rig. And Anthony DiFranco with the Open Insulin Project.
Here’s where things stand with those folks right now:
Adeline Umubyeyi has been doing less public advocacy since the pandemic started. Holding events where you gather lots of people — it’s just harder to do, and so are a lot of other things.
AND: She switched jobs. You might remember, this episode started with her talking about how even though she was working a professional job with decent insurance, she still had to ration insulin sometimes. To the point where she skipped meals to do it
The new gig has much better insurance. She has not had to worry about paying for insulin. She views it as a break, not a solution.
Adeline Umubyeyi Umubyeyi: God forbid, if I lost my job tomorrow, what am I going to do? You know, I would be a bright back in this same, in the same position.
Dan: She stays connected: Her bios on social media lead with “Type 1 diabetic,” “insulin for all.” That leads some people to seek her out for advice, which she’s happy to give.
Rogue Cowboy Hacker Terri Lyman says open-source tech for managing insulin and glucose levels has come a long way in the last year and a half.
For one thing, it’s more user-friendly than ever, including a smartphone app. So she spends less time guiding newbies through their setup.
Terri Lyman: I mean, it’s so easy to do. That you don’t really need somebody to help direct you through the documents anymore.
Dan: The new setups are also more sophisticated. They work with newer hardware— so she’s been able to replace her 2002 insulin pump with a new model, with a warranty and everything. And she doesn’t have to do as many manual adjustments.
Terri Lyman: I don’t think about diabetes very often, not nearly as much as I used to, if we could just get a cure and I can forget about it altogether and not spend the money, that would be even better.
Dan: Diabetes is STILL expensive. She has a steady job with good insurance, but she still hoards money and paid time off for equipment, and deductibles, and doctor visits.
And Anthony DiFranco, and the Open Insulin Project? Going strong. Anthony says They’ve been talking with regulators, and with legislators about how open-source insulin could be LEGALLY distributed.
Their plans sound more concrete and specific than before. Once the lab work is a bit farther along, they’re aiming to work with a contract manufacturer to get production going a little bigger and a little faster.
And: One of the lead collaborators moved to Baltimore and now has a grant for the city to start funding some of their work. Anthony estimates that producing usable insulin there would take a few years, and a few million dollars
Anthony DiFranco: So it’s actually remarkably practical to do, You know, start to finish it’s not a whole lot of money for a city or for a well-organized station group, you could put in a stretch of road, uh, in a small town for the same amount of money. Right.
Dan: Leslie Knope, if you’re listening…
Catching up with these folks got me thinking. A few weeks after we first published this episode, we decided to start focusing on self-defense. That became the theme of our third season, and in one episode, we profiled a person I called a medical-bill Ninja.
When that season ended, I started saying, Maybe we ought to build a dojo… a community of people, learning together and teaching each other. The pandemic gave us a lot else to chew on real quick, but IDEA of do-it-yourself, community self-defense— it’s been absolutely driving how I think about the show these days,
And now I’m like, HM. That medical-bill ninja, Meredith Balogh? She’s a type-one diabetic. Diagnosed as a kid.
I’m starting to catch on here that folks with Type 1 diabetes have been doing this for a LONG time, and on every level. Advocating. Sharing knowledge. Sharing INSULIN. And even building tech. And so much of it is self-organized.
Because of course: If you’ve got Type 1 diabetes, you’re up against everything that’s wrong with our health care system— literally every day, and it’s literally life or death. Anthony DiFranco was the last person I caught up with. I ran this observation by him, and he was like, YUP.
Anthony DiFranco: I think the fact that it is life and death for people who need insulin to survive has really focused us on this question of what do we do about it.
Dan: I don’t know where this observation leads exactly, except: it’s clearer than ever, there are a LOT more teachers, a lot more role models, who are a lot farther along, than I ever really imagined. And I just keep finding more. Which is good, because there’s a lot to learn, and a lot to do.
I’ll catch you in two weeks. Till then, take care of yourself.
this episode of an arm and a leg was produced by me. Dan Weisman edited by Whitney Henry-Lester in 2019. And by Marian Wang for this rerelease. Daisy Rosario is our consulting managing producer. Adam Raymonda is our audio wizard. Our music is from Dave Winer and blue dot sessions.
One more update. Avery Trufelman no longer lives in Oakland. She’s now in New York City, where she now hosts The Cut, a podcast from New York Magazine.
This season of an arm and a leg is a co-production with Kaiser health news. That’s a nonprofit news service about healthcare in America. It’s an editorially independent program of the Kaiser family foundation. Kaiser health news is not affiliated with Kaiser Permanente. The big healthcare outfit they share an ancestor, this guy, Henry J Kaiser. He had his hands in a lot of different stuff, like stuff, aluminum steel cars.
He poured concrete, like for the Hoover dam and a lot of basements in California. When he died more than 50 years ago, he left half his money to the foundation that later created Kaiser health news. You can learn more about him and Kaiser Health News at Arm and a Leg Show slash Kaiser.
Diane Webber is national editor for broadcast and Taunya English is senior editor for broadcast innovation at Kaiser health news.They’re editorial liaisons to this show.
Thanks to public narrative. That’s a Chicago based group that helps journalists and nonprofits tell better stories for serving as our fiscal sponsor, allowing us to accept tax exempt donations. You can learn more about public narrative at www dot public narrative dot org.
and as always, thank you to everybody who supports this show—and thanks to anybody who wants to join up at armandalegshow.com slash support.
Latest Episodes
Some more things that didn’t suck in 2025
How to pick health insurance — in the worst year ever
Some things that didn’t suck in 2025 (really)
Looking for something specific?
More of our reporting
Starter Packs
Jumping off points: Our best episodes and our best answers to some big questions.
How to wipe out your medical bill with charity care
How do I shop for health insurance?
Help! I’m stuck with a gigantic medical bill.
The prescription drug playbook
Help! Insurance denied my claim.
See All Our Starter Packs

First Aid Kit
Our newsletter about surviving the health care system, financially.